BHNS 2020 Journal Club
By L. Asfour
Ø Cochrane Review: Topical and Device based treatments for fungal infections of the toenails (January 2020)
· Foley K, Gupta AK, Versteeg S, Mays R, Villanueva E, Denny J.
Citation: Foley K, Gupta AK, Versteeg S, Mays R, Villanueva E, John D. Topical and device-based treatments for fungal infections of the toenails. Cochrane Database of Systematic Reviews 2020, Issue 1. Art. No.: CD012093. DOI: 10.1002/14651858.CD012093.pub2
Objectives
To assess the clinical and mycological effects of topical drugs and device-based therapies for toenail onychomycosis.
Selection criteria
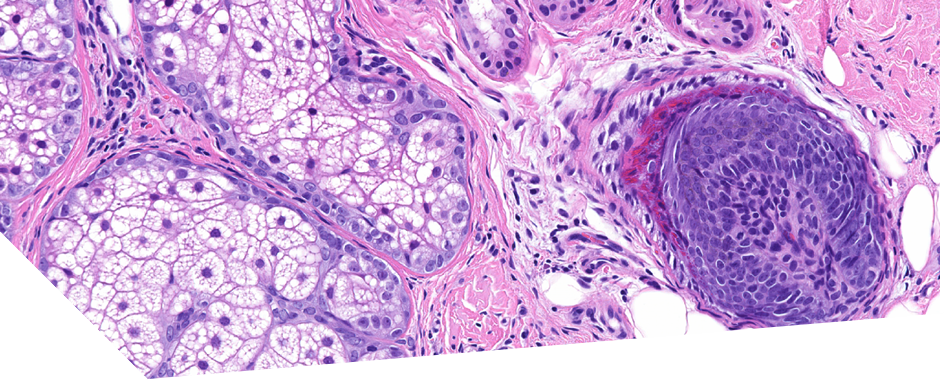
· Randomised controlled trials of topical and device-based therapies for onychomycosis in participants with toenail onychomycosis, confirmed by positive cultures, direct microscopy, or histological nail examination.
· Eligible comparators were placebo, vehicle, no treatment, or an active topical or device-based treatment.
· Primary outcomes were complete cure rate (normal-looking nail plus fungus elimination, determined with laboratory methods) and number of participants reporting treatment-related adverse events.
Results:
In searches up to May 2019:
· 56 studies including 12,501 men or women
· Average age: 27 to 68 years
· Mainly mild-to-moderate toenail onychomycosis. Onychomycosis duration was under-reported, but varied from months to years.
· Approximately 63% of the studies assessed onychomycosis caused by dermatophytes (fungi).
· Most studies lasted 48 to 52 weeks and were conducted in an outpatient setting.
On assessing complete cure:
· High-quality evidence supports the effectiveness of efinaconazole.
· Moderate-quality evidence supports P-3051 (ciclopirox 8% hydrolacquer) and tavaborole,
· Low-quality evidence supports ciclopirox 8% lacquer.
· Although evidence supports topical treatments, complete cure rates with topical treatments are relatively low.
· We are uncertain if 1064-nm Nd:YAG laser increases adverse events compared with no treatment or sham treatment (very low-quality evidence).
· Low-quality evidence indicates that there is no difference in adverse events between P-3051 (ciclopirox hydrolacquer), luliconazole 5% solution, and their comparators. Ciclopirox 8% lacquer may increase adverse events (low-quality evidence).
· High- to moderate-quality evidence suggests increased adverse events with efinaconazole 10% solution (commonly dermatitis and fluid-filled sacs) or tavaborole 5% solution (commonly, application-site reactions, such as dermatitis, redness, and pain).
· We downgraded evidence for heterogeneity, lack of blinding, and small sample sizes.
· There is uncertainty about the effectiveness of device-based treatments, which were under-represented; 80% of studies assessed topical treatments.
· Low- quality evidence from 3 studies compared laser to no treatment or sham treatment and there may be little or no difference in mycological cure. Complete cure was not measured, and we are uncertain if there is a difference in side effects between groups
Authors’ Conclusions:
Low evidence data overall. Future studies of topical and device-based therapies should be blinded, with patient-centred outcomes and an adequate sample size. They should specify the causative organism and directly compare treatments.