Management of Nail Psoriasis-
L Thomas, J Azad and A.Takwale
A review article summarizing management of Nail psoriasis based on anatomical involvement- Nail Matrix, Nail bed, Widespread nail involvement ( > 3 nails).
Each site has first , second line and third line treatment options. For Nail matrix the management described are: First line- IL steroids and others ; second line-Systemic therapy like Methotrexate, and third line- Biologics
For Nail bed the first line being Topical keratolytics and steroids; second line- systemic therapy and third line - Biologics as well.
The various topical therapies discussed include part from topical steroids, vitamin D analougue,
Topical retinoids, Tacrolimus and Intra lesions steroids.
Among the systemics options Cyclosporine and Acitretin are also included while mention of drugs such as Apremilast , Fumaric acid esters and others that may have some role in the management but not advised for nail psoriasis in particular have also been made.
Biologics especially TNF alfa, IL17, IL-12/23, antibodies have been mentioned as improving coexisting nail disease when prescribed for psoriasis and psoriatic arthritis without significant AEs.
Brief mention has been made of other clinical manifestations of nail psoriasis such as subacute or chronic paronychia which the proximal nail fold involvement which responds to topical steroids of high potency with antibacterial and anticandidal properties such as Dermovate NN(R) in the short term.Pustular nail disease
such as Acropustulosis lacks standardized treatment guidelines but use of Acitretin has been noted to be effective and rapid and sustained responses have also been reported with the use of anti-TNF agents , IL-1, IL-17& IL-12/23 inhibitors.
Lastly Nail psoriasis in children has been discussed. Management includes first line-
Avoidance of finger-sucking and wearing cotton gloves, Tacrolimus 0.1% ointment, Tazorotene 0.05% cream, vitamin D analogues on weekdays and topical steroids on weekend. Second line - systemic therapy and Third line - Biologics. These are attractive options in children as it requires less frequent laboratory monitoring and has more targeted action with less end organ toxicity. However there is a lack of long term safety data in children compared to adults and therefore at the moment only Adalumumab, Etanercept and Ustekinumab are licensed for children.
Inflammatory nail conditions. Part 1 : nail changes In psoriasis.
Part 2: nail changes in lichen planus & Alopecia Areata
P.D Yesudian & D. A.R. deBerker
This is another extensive two part review article on nail changes in psoriasis and in lichen planus and Alopecia areata providing brief summary of salient features in the clinical features, management & prognosis of these entities, with practical recommendations that may be benificial to all dermatologists.
Among the useful clinical features of nail psoriasis is the fact that Erythema in the proximal margin helps to distinguish psoriasis from other causes of onychomycosis.Splinter haemorrhages manifest as linear bleeds along the longitudinal axis of the nail plate, and are due to bleeding from dilated capillaries in the nail bed and are analogous to the Auspitz sign in the skin.
Clinical examination of nails can be done through the use of Dermoscopy; as a general rule set Dermoscopy is effective for nail-matrix changes and the use of gel under Dermoscopy is helpful for nail- bed changes. A range of splinter haemorrhage morphologies can be visualized. Pitting, onycholysis and salmon patches are also more clearly seen under the Dermoscopy.
The assessment of nail psoriasis can be made using the Nail Psoriasis Severity Index (NAPSI)
which is a semi objective way of assessing the nail changes in psoriasis. For each nail the score varies from 0 to 8 ( one point for every for both nail-bed and nail matrix involvement) with the total score varying from 0 to160.
Lastly management has been discussed in detail under the headings of general principles, topical agents, intralesional steroids, systemic agents and Biologic agents.
The general principles include the following-topical treatment can be helpful for limited disease. When topical treatments fail systemic or Biologics can be considered if > 3 nails are involved. If NAPSI is > or if patient quality of life (QoL) is significantly affected. Podiatrist can play an important role in shaping the deformed toenails affected by psoriasis.
When treating onychomycosis coexisting with psoriasis ( 20-25% of patients) care needs to be taken regarding interaction with antipsoriatic systemic agents, potential liver toxicity and increased potential for recurrence.
Among the Topical agents corticosteroids and calcipotriol are used most commonly. In RCTs
the use of topical betamethasone dipropionate ointment and calcitriol has shown beneficial effects on subungual hyperkeratosis , onycholysis and pitting.
In a randomized control open label study , topical tacrolimus administered as a 0.1% ointment demonstrated beneficial effects in both nail bed and nail matrix disease when used without occlusion for 12 weeks compared to controls.
Intralesional steroids in the form of intralesional triamcinolone (5-10 mg/dl) can be used monthly for 6 months to treat both nail bed and nail matrix. Alternatively a simplified protocol shown with a 3 monthly injection with triamcinolone acetonide (0.4mL, 10mg/dL) can also be followed. Adverse effects include pain, haematoma and nail- fold atrophy.
Methotrexate and dihydrofolate inhibitors are effective in mail psoriasis when used as an oral formulation or as a subcutaneous injection. A single- blind randomized study comparing methotrexate and ciclosporin revealed no statistical difference between the efficacy of both agents ( 43% and 37% improvement respectively in NAPSI at 24 weeks).
Acitretin has shown NAPSI improvement of 40-50% at 6-12 months, and is probably of particular use for thicker nails or for subungual hyperkeratosis.
Apremilast is a phosphodiesterase inhibitor that has showed significant improvement in NAPSI in trials (ESTEEM 1 and ESTEEM 2 -phase 11 RCTs) at week 16 & 32.
Tofacitinib is an oral Janus kinase inhibitor that is used for a variety of inflammatory dermatoses and at doses of 5 and 10mg demonstrated efficacy against placebo.All improvements were sustained at week 52.
The efficacy of Biologics in treating nail psoriasis has been well established by RCTs. They are divided into tumour necrosis factor alpha antagonists , interleukin (IL)-17 inhibitors and IL-23 inhibitors.
Anti TNF Alfa drugs include etanercept, adalimumab, infliximab and certolizumab pegol.
The efficiencies of the Biologics are as below-
Etanercept: the Target NAPSI improved by 29% at week 12 and 51% at week 54.
(CRYSTEL study)
Adalimumab in the post hoc analysis of the BELIEVE study showed median decrease in NAPSI by 39.5% at week 16
Infliximab in a randomised study has shown NAPSI improvement by 57.2% at week 24(P< 0.001%)
Certolizumab pegol in a double - blinded placebo controlled Phase 111 study (RAPID-PsA) showed
a mean NAPSI improvement by 36.5% at week 24 increasing to 64.5% at 48 months.
Secukinumab (at 300mg) showed an improvement in NAPSI upto 63.2% at week 32 in the TRANSFIGURE study.
Ixekizumab in the double blinded RCT (UNCOVER-3) showed a mean improvement in NAPSI of 36.7% at week 12 and > 80% at week 60.
Brodalumab has proved its efficacy in the AMAGINE studies 1,2&3. Ata dose of 219 mg it produced an improvement in NAPSI of 46.3% at week 12 compared with base line.
Ustekinumab has shown an improvement in NAPSI of 46.5% & 48.7% at week 24 at 45 mg and 90 mg doses respectively as seen in the PHOENIX study.
Guselkumab was compared with Adalimumab against placebo in the VOYAGE 1 trial focussing mainly on fingernail involvement. Improvement in target NAPSI was significantly better for Guselkumab compared to placebo at week 16
(mean improvement 37.5% vs 0.7%) and comparable to adalimumab at week 24.
Risankizumab was compared with Ustekinumab
in a comparative trial and showed more rapid nail improvement ( for example: improvement in NAPSI - 30% vs 0 at week 6).
No nail specific data is available at the moment for tildrakizumab.
Owing to different study protocols used in each trial, it is difficult to extrapolate data about the optimal Biologic agent for this condition.
Ixekizumab has the best mean NAPSI improvement at the 60 - week review , but data from other biologics for that time frame are not accessible.
Inflammatory nail conditions. Part 2: nail changes in lichen planus and Alopecia Areata.
Both are T cell - mediated inflammatory dermatosis of the Alim that frequently show nail changes.
Clinical features for Nail LP depends upon involvement of the nail matrix or the nail bed.
Nail Thinning, longitudinal ridging and distal splitting of the nail bed are the commonest clinical features.Trachyonychia, onychorrhexis,and red lunulae can also occur. Linear nail-bed dua HRI iA has been reported as a distinctive dermoscopic feature of NLP. Dorsal pterygium indicates late stage matrix involvement.
In children a retrospective study Torsi et al showed three different manifestations of NLP in children. First presentation includes nail ridging, thinning, splitting and dorsal pterygium. Second presentation in 20- nail dystrophy also called trachyonychia.The third variety is idiopathic atrophy of the nail, which is characterized by an acute onset and rapid course culminating in diffuse, painless nail destruction in a few months.
Less common presentation of NLP include bullous form with haemorrhagic lesions resulting in complete shedding of the nail plate with atrophy, splinter haemorrhages, koi limy hua and yellow nail syndrome-like changes.
Treatment
These are based on case series, expert opinion and case reports as no RCTs have been completed for this condition. Due to the slow growth rate a minimum of 3-6 months are required to evaluate any therapeutic intervention.
General measures include trimming of dystrophin nail plates, avoidance of excessive manicuring and optimal moisturizing of the nail folds.
Medical treatments can be divided into topical, intralesional and systemic therapies.
Topical steroids are the first line agents particularly for mild NLP. Tacrolimus 0.1% ointment has also been shown to be effective at a dose of twice a day in a small case series of five patients.
Intralesional triamcinolone are beneficial for Nail Matrix disease. In a prospective case series including 12 patients with NLP (monthly injections of 5mg/dl) had a 75-100% improvement. Currently the expert consensus is to use 5-10 mg/dl of triamcinolone depending on disease severity with a frequency of repeat injections every 4-5 weeks (changing to 6-8 weeks with improvement) for 4-6 months. Side effects include local atrophy including damage to the extensor tendon.
Systemic corticosteroids can be considered when > 3 nails are involved or there are signs of severe disease. Dose of oral steroids of 40 mg /day for 2 weeks followed by 30 mg/day for 2 weeks and intramuscular triamcinolone acetonide 0.5mg/kg/ month have shown efficacy.
In a long term retrospective case series of 75 patients with NLP treated with intralesional or systemic triamcinolone 27 patients were followed up for 5 years. 18 patients responded to the treatment and the other 9 did not.Of the 18 responders 11 developed a recurrence during the follow up.
Alitretinoin was used in 2 patients at a dose of 30mg a day for 9 months ; improvement was seen within 4 months in a case report. Other systemic agents used in this condition include - Azathioprine 100mg/day, ciclosporin 3-5mg/kg / day and mycophenolate mofetil 1g twice a day. Also low dose methotrexate 10-20 mg subcutaneously once weekly demonstrated improvement in two patients. A single case report of NLP responding to localised bath psoralen ultraviolet A was published recently.
Nail involvement in Alopecia Areata(AA) are more commonly seen in children (46% as per a study by Tosti et al) as they tend to develop more severe forms of AA (extensive hair loss, Alopecia universalis, Alopecia totalis).
Clinical features include pitting which tends to be smaller, shallower and regularly distributed with a grid-like pattern on the surface of the nail compared with psoriasis (Chelidze K. et al)
Other plate changes include trachyonychia, longitudinal ridging, punctate leuconychia, onychorrhexis, onycholysis and spotting of the lunulae (kasumagic-Halilovic E et al). Most changes are limited to nail matrix, while nail bed alterations such as onycholysis and subungual hyperkeratosis are exceedingly rare( Roest YBM et al)
Treatment is based on case reports as there are no RCTs or large scale case series available for this yet.
In topical therapy topical corticosteroids have been used to treat trachonychia. Mometasone furoate 0.1% ointment and betamethasone dipropionate 0.05% ointment for 6 and 10 months respectively have resulted in clinical improvement. A single case report of Tazarotene 0.1% gel every night for 3 months also conferred benefit.
Intralesional steroid/ triamcinolone 5mg/ml or 10 mg/ml used every 2-4 weeks for 2-3 months resulted in remission of pitting and trachyonychia,however, relapse occurred 4-6 months in ⅔ rd of the patients.To maintain the improvement it can be used for a longer period of time with increased treatment free intervals.
Systemic agents such as Tofacitinib (a Janus kinase inhibitor) has shown good results in case reports at doses ranging from 5-10mg/day for 4-10 months.
New effects of caffeine on the corticotropin-releasing hormone(CRH)- induced stress along the intrafollicular classical hypothalamic- pituitary-adrenal (HPA) axis (CRH-R1/2, IP3-R, ACTH, MC-R2) and the neurogenic non- HPA axis ( substance P, p75 NTR and TrKA) in ex vivo human male androgenetic scalp hair follicles.
T.W.Fischer & A. Bergmann et al
Translational message-
Stress can impair human hair physiology and induce hair loss.
Caffeine may effectively counteract stress- induced hair damage and possibly prevent stress- induced hair loss.
It has been already known that caffeine stimulates hair growth in male and female human hair follicles (HFs) in vitro.
This study for the first time documents the corticotropin- releasing hormone (CRH) induction of the hypothalamic -adrenal (HPA) stress axis in male Human HFs from biopsies (balding vertex area)
of men with androgenetic alopecia.
For the first time the non- HPA neurogenic stress axis has been shown in the same male human HFs.
Caffeine was shown to counteract both stress axes.
Lastly inositol triphosphate receptors was newly identified in human HFs.
Summary
Human scalp hair follicles contain a peripheral Neuro endocrine equivalent of the systemic hypothalamic pituitary adrenal (HPA) stress axis.
The objective of this research was to investigate whether caffeine would antagonize CRH- mediated stress in HFS.
HFs from balding vertex area scalp biopsies of men affected by AGA were incubated with CRH
with or without caffeine.
CRH , compared to controls, was found to significantly enhance the expression of catagen- inducing transforming growth factors- Beta-2 (p<0.001), CRH receptors 1 and 2 (p<0.001) and adrenocorticotropic hormone ( ACTH) (p<0.001%) melanocortin receptor 2 (<0.001%) and additional stress associated parameters , substance P and p75 neurotrophin receptor.CRH inhibited matrix keratinocytes proliferation and expression of anagen-promoting insulin like growth factor-1 (IGF-1) and the pro-proliferative nerve growth factor receptor NGF-tyrosine kinase receptor. Caffeine significantly counter acted all described stress effects and additionally enhanced inositol triphosphate receptor, for the first time detected in human HFs.
Conclusion.
These findings provide the first evidence in ex vivo human AGA HFs that the stress mediator CRH induces not only a complex intrafollicular HPA response, but also a non-HPA-related stress response. Moreover it was show that these effects can be effectively antagonised by caffeine. Thus, these data strongly support the hypothesis that stress can impair human hair physiology and induce hair loss, and the caffeine may effectively counteract stress-induced hair damage and possibly prevent stress- induced hair loss.
Psoriatic onycho- pachydermo-periostitis: a patient’s perspective
E.Forbat, M. Heath and T. N. Shim
Summary of Patient’s Viewpoint-
A young lady describes her patient journey of the
diagnosis of a rare and debilitating condition of her fingers nail of the right hand which started around September 2016.
Initially the little finger nail on the right hand started to lift off and later the same condition appeared on the left forefinger. The pain was excruciating. She says her ‘ once beautifully manicured fingernails now resembled deformed, callous , infected, badly swollen stumps”
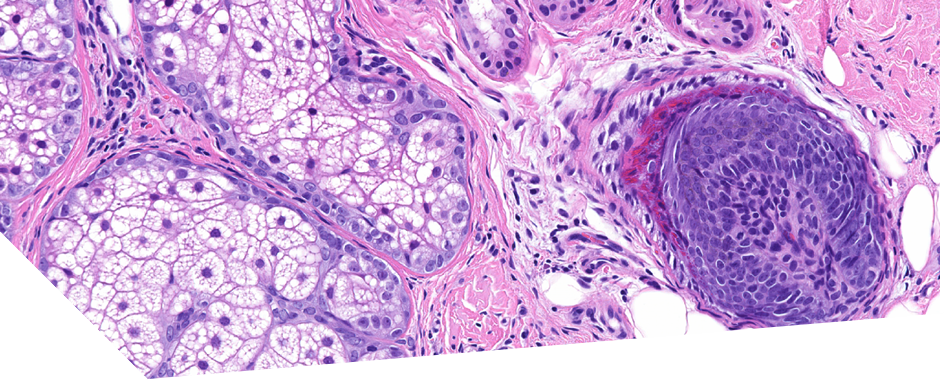
She describes how she had anticipated a cure and a quick fix in the first dermatology appointment but and upset when it did not match her expectations. She was almost in tears when she was faced with the prospect of going through it all again as the dermatologist requested for a nail clipping and even raised the possibility of skin cancer which she hadn’t thought of before. Long term acrylic nail use was also thought to be one of the possibilities. Subsequently she endured a distressing nail biopsy with the help of her husband and also had a patch test that showed allergy to cobalt and nickel but not nail acrylates.
She was invited to attend the Midlands Dermatology Society Meetings due to the complexity of her diagnosis. She was advised a second nail biopsy as the first one was inconclusive and cancer remained high on the list. She opted for a general Anaesthesia for her second biopsy which was done by a plastic surgeon.
The second nail biopsy rules out cancer. She had an X-ray of her fingers that showed some bony changes and subsequently a diagnosis of psoriatic onycho- pachydermo- periostitis was made.
She continues to suffer with recurrence of the callous on her two fingers and the thumb which is constantly painful with codeine and paracetamol are not helping .Simple tasks in public, such as putting items of shopping onto the conveyor belt at the supermarket have become embarrassing for her.Her daily life is restricted. Her husband helps her dress and she can no longer do household chores.
In the end she says that receiving a definite diagnosis was important for her even though there is no actual cure. She has been placed on methotrexate and folic acid for now and hopes that sometime in the future she will be free from this debilitating condition once and for all.
Summary of Clinician Comment
Psoriatic onycho pachydermo periostitis or POPP is an uncommon variant of psoriasis. It is characterized by psoriatic onycho dystrophy and is associated with onycholysis and connective tissue thickening above the distal phalanx with pathognomic radiological changes. These changes include Intra articular and periarticular erosions, periostitis, bony protuberance,soft tissue prominence (dactylitis and sausage digits)
and calcification at ligament and tendinous insertion in keeping with enthesopathy.
It’s the bone involvement in POPP which makes it a rare entity as opposed to the more common presentation of joint and nail involvement in Psoriasis.It may involve any nails but nails of the great toe are most commonly involved.
Treatment is challenging. Methotrexate is commonly used with variable success. It can be used alone or adjunctively with leflunomide or a biological treatment such as infliximab. Etanercept and Adalimumab have also been reported to have a favourable response.Our patient showed some clinical improvement on 15mg weekly maintenance dose of methotrexate.
She also finds adaptic digit dressings helpful.
Other options for treatment include combining methotrexate with leflunomide or Infliximab. Etanercept and adalimumab have also shown favorable responses.

Recommended Comments
There are no comments to display.