Onychoscopy in a columbian population with a diagnosis of toenail onychomycosis: an evaluation study for this diagnostic test
L.F. Gonzalez Cortes et al
Summary
This use of the dermatoscope has expanded beyond the diagnosis of the pigmented lesion to hair (trichoscopy) and nail examination(onychoscopy). According to the authors, this the first study using onychoscopy, as a potential diagnostic test for onychomycosis in a Columbian population while evaluating the sensitivity, specificity , PPV and NPV of the onychoscopy findings.
Methodology
In total 102 outpatients (69% women, 31% men; mean age 51.7 years) with confirmed onychomycosis (clinical diagnosis followed by positive direct microscopy with KOH or fungal isolation by culture, with exclusion of patients with a history of psoriasis and lichen planus), underwent onychoscopy by 3 separate consultant dermatologists.
Results
The onychoscopy findings were: longitudinal striae, distal spiked pattern, distal irregular termination, linear edge and ruins aspect.
A statistically significant association was found between the clinical symptoms of onychomycosis and both the clinical feature of dyschromia (OR=3.99; P<0.05) and the onychoscopy feature of longitudinal striae (OR=4.7;P<0.05). Further analysis and results of the sensitivity, specificity,PPV and NPV of all onychoscopic findings were presented in a tabular form (main article).Linear edge on distal nail plate was a finding in traumatic onycholysis and useful in differentiating from Onychomycosis (specificity=84.9% and PPV=80% got onychomycosis)
Limitations
PAS staining which is considered the gold standard of diagnosis for onychomycosis was not utilised. Convenience sampling was adopted as opposed to Random sampling. The study number was small and no associations between the clinical and onychoscopiy findings with the different fungal species isolated were explored.
Conclusion
The authors acknowledge the diagnostic challenge for onychomycosis owing to variable sensitivity and specificity of the current diagnostic techniques (KOH examination= sensitivity of 53%-76% and specificity of 38%-8% ;fungal culture=high false-negative rate upto 60% and histopathological examination with periodic acid-Schiff staining has a sensitivity of 62% though a high specificity of upto 100% than either KOH preparation or culture alone. But although it will demonstrate fungus it’s not cost saving and sometimes a painful and uncomfortable procedure for patients).
They present and reinforce -other previous studies- onychosopy as an alternative method for diagnosing this common dermatological condition given it is cheap, straightforward and also has the potential to differentiate onychomycosis from traumatic onycholysis.
Assessment of nail findings in children with atopic dermatitis S. Atalanta Uku et al.
Background:
The authors have attempted to perform nailfold capillaroscopy in children and determine it’s association with atopic dermatitis (AD) and it’s severity.
Methodology
100 participants between 2-16 years were divided into 50 with the diagnosis of AD according to the Hanifin-Rajka criteria and the other 50 healthy controls without AD. The AD severity score (SCORing Atopic Dermatitis: SCORAD) was calculated for all patients with AD.
A digital epiluminescence device was used for nailfold capillaroscopy by a single user for consistency.The middle of the nail was examined separately from the edges due to the curvature of the nails. Those with local trauma or thick nailfold skin were not evaluated.
The authors used the predetermined criteria for scleroderma as there are no capillaroscopic evaluation criteria for nailfold examination in patients with AD, as yet.
The capillaroscopic changes of the participants in terms of capillary dilatation, irregularity in capillary array, capillary dilatation, capillary morphology including tortuosity (folding), ramification (regular branching), bush-like( irregular branching), capillary haemorrhage and avascular areas were examined. A capillary density of more than or equal to 7mm was considered normal.
For statistical analysis differences between groups were assessed using Student t-test for parametric data and Chi-square test for non parametric results.
Results
Capillaroscopic examination of children with AD revealed significant pitting, capillaroscopic findings including a decrease in capillary density, irregularity in capillary array, capillary dilatation, tortuosity, ramification increase, bush like appearance and avascular areas. SCORAD was also associated with nail changes.
Conclusion
The nailfold capillaroscopy results in children with AD showed similarity to those patients with scleroderma spectrum disorder. Moreover, the authors note that the correlation between clinical and capillaroscopy findings varied hence the need for a detailed clinical examination of patients.
Erythema Nodosum in patients with kerion of the scalp N.Ben Salah & M. Korbi et al.
The authors report 3 cases of a rare presentation of Erythema Nodosum (EN) as a dermatophytid reaction to tinea(kerion) of the scalp.
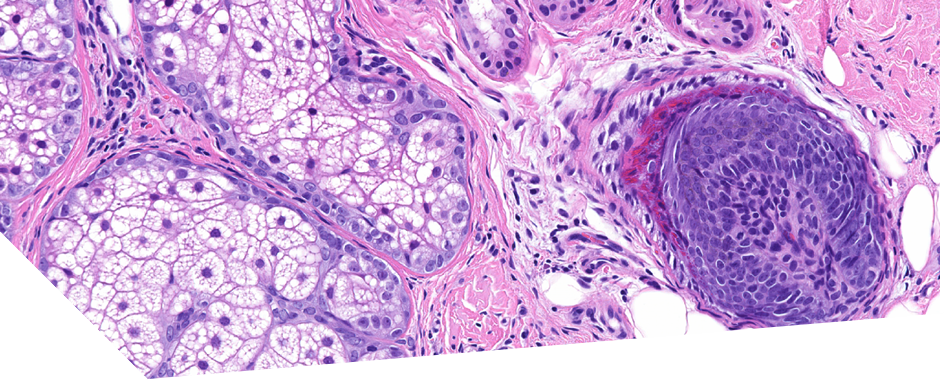
Three boys presented with patches of hair loss associated with pustular lesions on the scalp. Mycological examination confirmed the diagnosis of kerion. A few days after the onset of oral therapy with griseofulvin the patients presented with painful erythematous papulonodular lesions on their legs which were clinically consistent with EN. A diagnosis of EN- type dermatophytid reaction was made for each of the three cases. Treatment with griseofulvin was continued and the lesions of EN on all cases resolved spontaneously without sequelae.
The above diagnosis was made based on the three diagnostic criteria proposed for this in the literature:
1.proven dermatophytid infection
2.distal eruption in the skin free of fungal organisms and
3.resolution of the dermatophytid with antifungal therapy
The two possible underlying theories for the pathogenetic mechanism for this eruption are:
1.antigen-antibody reaction and immune complex deposits around the septa of the hypodermis
2. due to a type 1V hypersensitivity reaction to the released antifungal antigens from the site of infection.
In conclusion, the authors suggest that the EN can be a dermatophytid reaction secondary to the tinea infection of the scalp. As this association is rare it can be interpreted as an allergic reaction to the antifungal medication, however, as demonstrated in the above case they emphasise that therapy should be continued even after the development of the dermatophytid reaction.