CED
Therapeutic experience with oral finasteride for androgenetic alopecia (AGA) in female-to-male transgender patients. O. M. Moreno-Arrones, A. Becerra, S. Vano-Galvan. CED 2017; 42:p743-748
In some transgender men, exogenous testosterone administration acts as a trigger for male-pattern alopecia. This study aimed to describe the clinical characteristics of transgender men affected with AGA and to evaluate the effectiveness and safety of treatment with the oral type II 5α-reductase inhibitor, finasteride. The study enrolled female-to-male transgender patients with a clinical diagnosis of AGA who had received finasteride 1 mg daily from 2014 to 2016. All patients were being treated with testosterone 1000 mg IM every 3 months. In all, 10 patients (mean age 35 years) were included in the study. The mean onset of AGA was 3.25 years after the introduction of androgen treatment. Interestingly, 70% of the patients had a family history of AGA, and this subgroup of patients developed AGA approximately 1 year earlier than the remaining patients. All 10 patients had received a clinical diagnosis of male-pattern AGA with 9 (90%) classified as stage IV on the Norwood Hamilton (NH) scale at the start of finasteride treatment, while the remaining patient had stage III disease. All the patients improved one grade on the NH scale after a mean of 5.5 months from the start of finasteride treatment. Three patients stopped treatment and, it was noted that their alopecia improvement completely reverted on average 4.3 months after cessation of finasteride. No other adverse effects were noted. Mean follow-up of patients was 16.2 months (range 12–26 months).
Their data suggested that testosterone-induced alopecia in transgender men behaves clinically and therapeutically as common male-pattern AGA in cis-gender men i.e. similar frontotemporal follicular regression pattern, dermoscopic signs and favourable response to daily oral administration of finasteride. Also, low levels (1 mg) of daily finasteride (which lowers serum and scalp DHT levels by > 60%) were enough to clinically improve the alopecia, but also, did not alter the serum testosterone levels in the transgender men. The authors recommended waiting until the patient has acquired the desired secondary sex characteristics and testosterone levels are within the recommended range before starting treatment with finasteride 1 mg for AGA. They also proposed new nomenclature for classification of AGA in transgender patients i.e. ‘female-to-male androgenetic alopecia’ (FtM-AGA) to refer to the onset of AGA in transgender men, which can present either as a male (FtM-AGA-M) or female pattern (FtM-AGA-F). In transgender women, similar nomenclature can be used (MtF-AGA-M/F). They acknowledged the main limitations of the study, which were its small sample size and short-term follow-up of patients.
For each patient, we collected epidemiological data, personal and family clinica l history, hormonal analytical values [testosteron e, oestradiol, s ex hormo ne-binding globulin (SHBG), luteinizing hormone (LH) and follicle-stimulating hormone (FSH), whole-blood haematological and serum biochemical values (haematocrit, bio-chemistry, hepatic enzymes, and levels of lipidn ferritinand thyroid hormone). Clinical and trichoscopic examination was performed at each visit. Alopecia wasnmeasured by the Norwood–Hamilton (NH) scale for male-pattern AGA. The patients continued under follow-up by the endocrinology department for clinical (blood pressure, body mass index and evaluation of Ferriman–Gallwey score), analytical, hormonal and radiological (bone densitometry and mammogram) evaluations. Clinical improvement was defined by a decrease in stage on the NH scale. Sexual desire was evaluated using a visual analogue scale (VAS). Each patient was asked to evaluate his sexual desire from 0 (no desire) to 10 (strong desire) responding to the question ‘When you have sexual thoughts, how strong is your desire to engage in sexual behaviour with a partner?’ at the screening visit and after 1 year of treatment. Continuous variables are presented as mean values and minimum and maximum ranges, and categorical variables are presented as absolute numbers and percentages.
Lichen planopilaris in Latin American (Chilean) population: demographics, clinical profile and treatment experience. F. Mardones, J. Shapiro CED 2017; 42:p755-759.
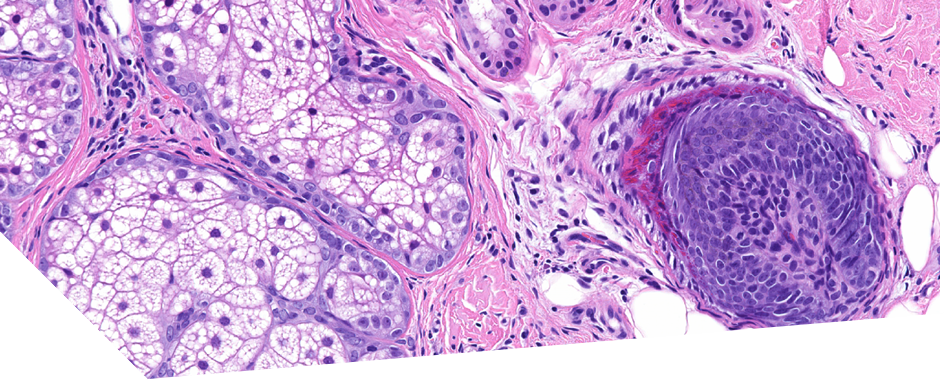
Lichen planopilaris (LPP) is an uncommon chronic inflammatory hair disorder that may induce hair loss and scarring alopecia. The authors noted that epidemiological studies on LPP are limited from certain geographic areas and, that racial and ethnic differences have not been fully investigated to date. In this study, the authors looked to obtain information on demography, clinical profiles and treatments used in Chilean adults with LPP. They gained information from the medical records of adult Chileans with a clinical and histological diagnosis of LPP from 2010 to 2014 from the Dermatology Department of the University of Chile Clinical Hospital and from a private practice. Treatment response was clinically recorded as: no response, mild (≤ 50%) improvement or satisfactory (> 50%) depending on the intensity of reduction/absence of inflammation or hair loss. In total, the study assessed 103 patients [67 women (mean age 54.1 years) and 36 men (mean age 39.1 years)]. Of the 103 patients, 75 (72.8%) were diagnosed with classic LPP (CLPP). It was noted that there was a statistically significant sex difference in age of onset, with men having onset at a significantly (P < 0.001) younger age. Frontal fibrosing alopecia (FFA) was observed in 27 patients (26.2%) i.e. 26 women (mean age 62.9 years) and 1 man. They found only one case (1%) of Graham–Little–Piccardi–Lasseur Syndrome (GLPLS), which was a 50-year-old man. In this study, the incidence of concomitant disease was high (mostly hypothyroidism, hypertension and metabolic disorders), however, there were no age-matched controls. Depression was also a common finding in patients with CLPP. In this investigation, scalp dysaesthesia (itching, tenderness and burning sensation) was more common in CLPP (88%) than FFA (30%). In this study, the majority of patients with CLPP had inflammatory signs in the vertex area but almost 30% had a more disseminated condition. Additionally, 41% had small localized cicatricial patches and 27% had large and coalescent patches at the time of diagnosis. In FFA, all of the patients had band-like scarring on the hairline margins of the scalp. Unlike previous reports, only 2.7% of the patients had lichen planus-like lesions in other body areas, mostly on the face and axillae.
Regarding topical treatment, clobetasol 0.05% foam or lotion was used by all patients, while minoxidil 2–5% lotion was used by 16 patients (21.3%) with CLPP and 15 patients (55.6%) with FFA. Salicylic acid 1% lotion was used by 52 patients (50.5%) with LPP. As for systemic treatment, 15 patients (20%) with CLLP and 7 (26%) with FFA were treated with hydroxychloroquine 200–400 mg/day; 10 patients (13.3%) with CLPP and 8 (29.6%) with FFA were treated with finasteride 1–2.5 mg/day; and 9 patients with CLPP had other treatments including methotrexate and isotretinoin. After 12 months of treatment, none of the patients had achieved complete clinical remission. Mild and satisfactory improvement results were recorded for 49 (65.3%) and 20 (74.1%) cases of CLPP and FFA respectively, and 26 (34.7%) patients with CLPP and 7 (25.9%) with FFA were categorized as progressive nonresponders. They concluded that the best approach and treatment regimen for LPP was still uncertain. However, expert recommendations for CLPP and FFA are similar, and include topical steroids and/or tacrolimus, intralesional steroids, or minoxidil as first-line therapy for acute, small and circumscribed lesions. For patients who respond poorly to these or have an extensive rapidly progressive condition, systemic drugs (corticosteroid, doxycycline, hydroxychloroquine, ciclosporin, mycophenolate mofetil, oral retinoids and peroxisome proliferator-activated receptor-γ agonists) may be indicated. Additionally, benefit from 5α-reductase inhibitors (finasteride and dutasteride) has been reported in FFA. In their local treatment protocol, they preferred topical clobetasol 0.05% in shampoo or lotion over intralesional corticosteroid as it was better tolerated and shown to be effective. In almost a third of the cases (mostly FFA), 2% or 5% minoxidil lotion was also required.
Painful nails and white macules. A. Le, B. Richert, U. Sass et al. CED 2017; 42: p817-819
This was a clinicopathological case in the CPD section of the journal. A 36-year-old African woman presented with painful nail alterations, predominantly on her fingers. On examination, she was found to have longitudinal melanonychias, a splinter haemorrhage, a V-shaped notch in the free edge of the nail, and thin and wide longitudinal leuconychias; in addition, the nail on the left index finger was more severely dystrophic. The leuconychias had been present since puberty, while the more severe nail dystrophy of the index finger had been present for 2 years. The patient also had a profusion of tiny asymptomatic hypopigmented macules on her trunk, thighs and upper arms, which had progressively appeared since childhood. She reported that her grandmother and mother had similar cutaneous lesions but no nail alterations. No other skin lesions were seen. Punch biopsy from the distal nail bed area revealed a focal suprabasal epidermal cleft, a multinucleated keratinocyte, a dyskeratotic cell and a discrete mononuclear perivascular inflammatory infiltrate in the superficial dermis. PAS showed numerous pseudohyphae and Candida albicans grew on culture.
In this patient, the presence of suprabasal acantholysis associated with nail alterations and confetti-like leucoderma was consistent with Dariers disease (DD). Nail alterations are seen in up to 99% of patients with DD usually manifesting after the age of 5 years and consisting of longitudinal red and/or white lines extending from the base of the nail across the lunula to the free margin, along with nail fragility, V-shaped notches at the free edge, longitudinal ridging, painful splitting and subungual hyperkeratosis. The toenails are less often and less severely involved than the fingernails. Dermatophytes such as Candida or Pseudomonas often contaminate abnormal nail plates, as in this case. The presence of guttate leucoderma is an unusual clinical presentation of DD with about 35 reported cases, all in patients with dark skin phototypes.
BJD
In this month’s issue of the BJD there were no relevant research articles. There were 3 brief articles in the Image Correspondence section related to hair and nail disease with interesting images available to view.
Image Gallery: Nail involvement in syphilis: the great forgotten. Fusta X et al. BJD (2017); 177: p e158
This was a case report of a 36-year-old male with untreated HIV infection that presented with fever and a 2-month history of erythematous scaly plaques affecting his palms and soles. All nail plates showed Beau’s lines, distal amber discolouration and onychomadesis. Treponemal and non-treponemal tests confirmed the diagnosis of secondary syphilis. Normal nail regrowth was observed after penicillin treatment. The authors reminded us of the need to consider syphilis in the differential diagnoses for particular nail changes.
Image Gallery: Dissecting cellulitis (DCS) of the scalp following anabolic steroid use. Kurtzman D.J.B. et al. BJD (2017): 177: p e160
This was a case report of a 38-year-old man with the abrupt onset of DCS shortly after starting to take anabolic steroid for recreational performance enhancement. The patient showed marked improvement after cessation of anabolic steroids and commencement of isotretinoin 0.5mg/kg/day. The authors suggested that this case supports the distinct role of androgens in the pathogenesis of this condition.
Image Gallery: unusual images of monilethrix: the eyebrows and the biopsy. Anzai A et al. BJD (2017); 177: p e163
This was a case report of a 30-year-old patient exhibiting sparse scalp and eyebrow hair since birth. She had an aunt with similar features. Scalp examination revealed non-affected hairs alongside short and broken hairs, and keratotic pigmented papules mainly involving the occiput. Nails and teeth were normal. Trichoscopy of the scalp and eyebrows and optical microscopy revealed regular constrictions of the shaft, giving the characteristic beaded appearance of monilethrix.
JAAD
Frontal fibrosing alopecia (FFA) among men: A clinicopathologic study of 7 cases. Tolkachjov S.N., Chaudry H.M., Camilleri M.J. et al. JAAD Oct 2017; 77(4): p683-690
This is a retrospective study that aimed to characterise the clinicopathological findings of FFA in males. FFA was first described in postmenopausal women by Kossard et al in 1994 and, in males, is rarely reported in the literature. The authors conducted a retrospective review of all cases of male patients with FFA at the Mayo clinic from 1992 to 2016. Patients were included if they had a clinical diagnosis of FFA or a diagnosis of lichen planpilaris (LPP) with distribution in typical FFA sites. Response to treatment was classified as: unaltered disease progression, slowing of disease progression and disease stabilisation. In total, they identified 7 male FFA patients with a mean age at diagnosis of 54.6 years. The frontal scalp (6/7 patients), sideburns (4/7 patients) and temporal scalp (4/7 patients) were most frequently involved. 3 patients had involvement of the eyebrows. 1 patient had hair loss from the upper cutaneous lip. All patients had evidence of LPP on scalp biopsy. None of the patients had associated autoimmune or thyroid disease. Two patients had hypogonadism upon testosterone studies. Initial treatment recommendations were solely topical in 5 of 7 patients but, ultimately 4 of 7 patients commenced systemic treatment. Disease stabilisation was documented in 3 patients following treatment with hydroxychloroquine, after an average of 131 days. They concluded that the demographics of their male FFA cohort were similar to previously reported cases of FFA in men. The authors also proposed a classification system to improve recognition of FFA in men, which included features described by Kossard et al, as well as other associated sites identified in this study such as sideburns and facial hair loss. They also noted that FFA may be present without classical involvement of the frontotemporal hairline, and that isolated thinning or loss of eyebrows may assist in distinguishing FFA from androgenetic alopecia. Finally, they acknowledged that the small study size and incomplete follow-up data limited the ability to extrapolate data from this study and that larger studies were necessary to confirm findings.
Yellow facial papules associated with frontal fibrosing alopecia (FFA): A distinct histologic pattern and response to isotretinoin. Pedrosa A.F., Duarte A.N., Haneke E. et al. JAAD 2017; 77(4): p764-766
This is a retrospective cohort study describing the presence of yellow facial papules, a novel clinicopathological feature of FFA, and their response to treatment with isotretinoin. FFA was first described in 1994 and, since then, additional clinical features have been included in its definition including eyebrow loss, occipital and body hair involvement, glabellar red dots, visible frontal veins, and facial papules. Facial papules have previously been described associated with a lichenoid inflammation involving vellus hair follicles and perifollicular fibrosis. Recently, a series of 12 cases reviewed FFA facial lesions and reported that these apparently noninflammatory papules were depicted in 11 of 12 patients (91.7%) and displayed the aforementioned histologic features.
Of 108 patients with FFA followed at a single dermatology center between January 2009 and December 2016, 62 patients exhibited yellow facial papules. From this sample, the authors reviewed 10 cases including 9 white women (6 premenopausal) and 1 man, with a mean age of 44.5 years and a median duration of FFA of 12 months. Yellow papules were found on the temporal area (n=3), cheeks (n=1), chin (n=2), or diffusely distributed throughout the face (n=4). Histopathologic findings were found to be similar, with hypertrophic sebaceous glands in the papillary dermis with no associated vellus hair follicle or lichenoid inflammation, leading the authors to hypothesize that inflammation eventually resulted in the loss of vellus hair follicles which were replaced by fibrous scar tissue, whereas the hypertrophic sebaceous glands still remained, giving the clinical appearance of yellow noninflammatory papules on the face devoid of terminal hairs.
The authors used oral isotretinoin, 10 mg every other day, to their usual treatment regime for FFA (finasteride 2.5- 5 mg/day or spironolactone 25-50 mg/day for females and vitamin supplements plus pimecrolimus cream) for these 10 patients with FFA. They describe a visible reduction of the yellow facial papules associated with an improvement of skin ‘‘rough- ness’’ reported by the patients after a median time of 2 months and clinically observed after a median time of 4 months This treatment was usually extended for at least 12 months, with no reports of hair loss increase.
They concluded that the novel histologic finding of yellow facial papules in FFA, probably represents an intermediate step between the initial lichenoid inflammation and the ultimate skin atrophy without hair follicles and that low-dose isotretinoin could be a valuable option to improve cosmetic appearance in these cases.
Lack of efficacy of apremilast in 9 patients with severe alopecia areata (AA). Lucy Y. Lui, Brett A. King. JAAD Oct 2017; 77(4): p773-774
This is a letter to the Editor summarising a small research study investigating the potential use of apremilast as a treatment for AA. Based on previous mouse models of AA, suggesting that IL-15 and IFN-γ may be important in the pathogenesis of AA, the authors hypothesised that apremilast could be a useful treatment option in this condition, via suppression of IFN-γ. Furthermore, in a previous study using a humanised mouse model of AA, treatment with apremilast had resulted in prevention of hair loss. In total, 9 consecutive patients with severe AA (>/=50% scalp hair loss) or alopecia universalis (AU) were treated with oral apremilast 30mg bd for 3-6 months (mean 4.2 months, SD 1.2 months). There were 5 female and 1 male patient in the study. One participant had AA and the rest had AU, with a mean disease duration of 23.3 years. All had previously failed other therapies including tofacitinib, steroids and topical immunotherapies. They used the Severity of Alopecia Tool (SALT) to measure and assess treatment response. In summary, they found that no patients experienced any significant hair regrowth over the treatment period and apremilast was not shown to be of any clinical benefit. The authors hypothesised that differences between human disease and mouse models of AA, and/or the relatively short treatment duration, may have contributed to the lack of effect seen and, that the results of an ongoing larger study examining the effect of apremilast in AA were needed.
JID
This month’s edition of JID, included several late-breaking abstracts from the Society for Investigative Dermatology 2017 Annual meeting, summarised below:
1. Follicular regeneration in response to wounding in CCCA. N. Clemetson et al. JID 2017; 137: B12
Central centrifugal cicatricial alopecia (CCCA) is an inflammatory condition that causes permanent scalp alopecia in black women. Treatment options are limited. Wounding has been shown to generate hair follicles de novo, likely under the influence of Wnt signaling. Ablative carbon dioxide (CO2) laser therapy creates small wounds in the skin. In this exploratory study, we hypothesized that follicular regeneration in CCCA may be demonstrated by increased scalp hair counts, in response to wounding with a CO2 laser. We enrolled 17 women with CCCA, age 18+ years and treated two areas of the scalp with a fractionated CO2 laser. Pulse energy was 55mJ, 110mJ or 240mJ. Each subject was her own control, using a split scalp model. Photographs and punch biopsies were obtained. The difference in hair counts (from baseline to final visit) was calculated and compared using the Wilcoxon signed-rank test. From the baseline to final visits, average hair counts increased 73% vs 48% in peripherally treated vs untreated areas. Hair counts increased 66% vs 49% in centrally treated vs untreated areas. At 240mJ, the increase in hair counts in treated vs untreated peripheral areas was significant (p=0.03). Centrally, there was no significant difference at all pulse energy levels. While the general trend was toward an increase in hair counts in all areas, the most significant change was noted at peripheral sites treated at the highest energy setting. These findings support our hypothesis that follicular regeneration may occur in CCCA in response to wounding.
2. Role of transcription factor Ovol2 in skin epithelial regeneration and repair. D. Haensel et al. JID 2017; 137: B12
Epithelial cells possess the ability to become mesenchymal cells under appropriate conditions. Complete epithelial-to-mesenchymal transition (EMT) generates crucial cell types such as mesoderm and neural crest during embryogenesis, whereas partial EMT underlies pathological processes such as wound healing and cancer metastasis. Whether and how EMT impacts the self-renewal and differentiation of adult epithelial tissue stem cells is not clear. We had previously identified zinc finger transcription factors Ovol1 and Ovol2 as critical inhibitors of EMT during skin and mammary epithelial morphogenesis. Here we investigate the role of Ovol2 in adult skin epithelial regeneration and repair, and its possible connection to EMT regulation. We show that Ovol2 is expressed in adult epidermal basal and hair follicle bulge cells as well as their early progenies. K14-Cre-mediated deletion of Ovol2 delays hair follicle anagen progression and epidermal wound healing. Ovol2-deficient adult epidermal cells show reduced hair regenerating capacity upon transplantation, and display aberrant dissemination behaviors when they migrate to repair cutaneous wounds. FACS analysis reveals a decreased number of hair follicle stem cells (HFSCs) in skin from adult mice lacking Ovol2, and gene expression analysis reveals enhanced EMT and de-enhanced cell cycle gene signatures in Ovol2-deficient keratinocytes. Without Ovol2, HFSCs display mesenchymal-like morphology, defective clonal growth, and altered cell division behavior accompanied by an apparent cell cycle arrest between G2/M and G1. Ongoing experiments address the potential molecular mechanisms underlying these regeneration/repair and cellular defects, and data will be presented.
3. Differentiation of dermal papilla cells into a myogenic lineage for the treatment of duchenne muscular dystrophy. M. Rashidi et al. JID 2017; 137: B12
Duchenne muscular dystrophy (DMD) is the commonest muscular dystrophy caused by the absence of dystrophin. Stem cell therapy in DMD is one of the promising approaches for treatment. Multipotent stem cells residing in the hair follicle papilla are highly plastic. We showed that dermal papilla cells (DPC) undergo myogenic differentiation when co-cultured with different types of myoblasts including dystrophic human myoblasts. DPC incorporated into myotubes and upregulated the muscle marker, myogenin, in the co-culture with human myoblasts. DPC incorporation efficiency was low (< 5%) in all co-cultures and differed significantly (p value ≤ 0.001) between various types of myoblasts; however, no significant difference was observed between normal and dystrophic human myoblasts (p value ≤ 0.001). These encouraging findings suggested that the altered properties of dystrophic human myoblasts did not compromise the myogenic differentiation of DPC in vitro, supporting their in vivo application and possible therapeutic potential. The in vitro effects of galectin-1 and activation of Shh signaling pathway via recombinant Shh (rShh) and purmorphamine, on the myogenic differentiation of DPC, was also evaluated. None of the treatments increased myogenin expression in DPC; but, triggering Shh signaling produced a dose dependent pattern whereby the lower levels of signaling promoted myogenic differentiation while the higher levels inhibited it. Activating Shh signaling upstream of Smo, via purmorphamine, induced a biphasic differentiative response; however, the application of rShh hindered the differentiation of both cell types. Thus, murine DPC are a readily accessible source of stem cells that can undergo myogenic differentiation in vitro and their myogenic differentiation can be enhanced with proper treatment.
4. In vitro examination of Mexican hair shaft morphology using optical coherence tomography. M. Perper et al. JID 2017; 137: B12.
Hair diameter, shape, mechanical properties, combability, and moisture content have been previously examined, however primarily in Caucasian, African, and Asian individuals. We describe the distinct cross-sectional and morphological hair characteristics of Hispanics, an ethnic group accounting for 16% of total hair product sales in the United States, yet one that is not sufficiently studied. The VivoSight® swept-source multi-beam optical coherence tomography (OCT) system was used to evaluate hair diameter and shape in 30 female volunteers aged 18 to 55 recruited from Hospital Médica Sur in Mexico. Three hair samples from each volunteer were measured transversely along three distances, generating 9 cross-sectional images, 2 measurements per image, and 18 measurements per patient for a total of 540 diameter measurements in 30 patients. Samples were measured 10 mm from the proximal portion of the fiber, middle position (equidistant point between the root and end), and 10 mm from the distal portion of the fiber. The minimum hair diameter of all measurements (n = 540) was 0.06 mm while the maximum was 0.14 mm. The mean diameter of the hair samples was 0.10 ± 0.01 mm. Of note, we found that Mexican hair resembles Caucasian and Asian hair, in that hair shafts tend to be round-shaped with homogenous diameters throughout the fiber, rather than elliptical, flattened, and irregular, as seen with Afro-ethnic hair. Mexican hair is similar to Asian hair in terms of diameter and shape, and thicker on average than Caucasian hair. Our findings suggest that OCT may be a viable method of hair examination in addition to more traditional approaches such as light, confocal, scanning electron, and transmission electron microscopy. Retailers may use information garnered from this study to tailor hair products to the unique hair characteristics of Hispanics, an ethnic group driving sales in the hair care market.
JEADV (no Oct issue available) JAMA Dermatology
The Linear Nail Streak: A Lesson in Cultural Humility. Neil S. Prose. JAMA Dermatol Oct 2017;153 (10): p1064- 1065
This was a humorous letter to the Editor citing an unusual yet interesting case! The author had been reading The Mercury (the leading daily newspaper in Durban, South Africa) and noticed a photograph of an individual with a dark streak on his thumbnail on the front page. The linear streak of color extending from the nail bed, matrix, and nail plate to the adjacent cuticle and proximal nail fold, widely known as Hutchinson sign and suggestive for subungual melanoma. The author contacted the newspaper editor in the hope that the person whose thumb was pictured in the photograph could be identified and referred for medical attention. Initially, the editor shared his concern and offered to track down the photographer and the man in the photograph. Five minutes later, the editor called back to ask me if it was possible that I was referring to the ink mark on the thumb that all voters receive to show that they have voted. I sheepishly said that it might well be the case. Shortly after, his mother-in-law returned from the local voting center, and after he examined her left thumb he concluded his research!
Interestingly, the author informs us that electoral ink, also known as voter’s ink and election stain, is used in many countries to prevent double voting. It is a silver nitrate compound that is applied with a marking pen, staining the skin on exposure to UV light. On the cuticle, the ink is particularly difficult to remove, lasting for 2 to 4 weeks. In a recent study, researchers in India were able to use the voter’s ink that was placed on Election Day to study the average rate of nail growth among patients at an outpatient clinic. The author reminds us about the importance of evaluating physical findings in the light of their social context and reminding us that dermatologists may also encounter this phenomenon when examining patients who have recently voted in their country of origin.