HAIR AND NAIL PAPERS – DECEMBER 2017
BJD
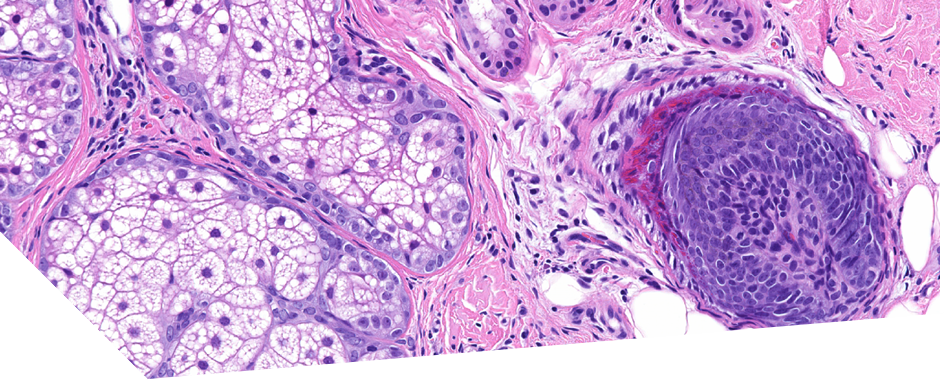
Cover Image: Trichophyton violaceum destroys hair keratin fibres in tinea capitis(pages 1767–1768)
K. Zhuang, X. Ran and Y. Ran. Version of Record online: 8 JAN 2018 | DOI: 10.1111/bjd.15984
This is the cover image of the December BJD and shows the arthrospores of Trichophyton Violaceum invading the cortical layer of hair in a 9 year old boy with black dot ringworm under scanning electron microscopy. The organism is gradually destroying the normal structure of the hair shaft by degrading the keratin fibril bundles into macrofibril fragments, which can be further assimilated for its proliferation.
Heterogeneity of trichoscopy findings in dissecting cellulitis of the scalp: correlation with disease activity and duration (pages e331–e332) A.E. Verzì, F. Lacarrubba and G. Micali. Version of Record online: 16 NOV 2017 | DOI: 10.1111/bjd.15685
This research letter reports the trichoscopy findings of 6 white men (mean age 31 years, range 23–37) with dissecting cellulitis of the scalp of at least 1 year’s duration and their correlation with disease activity and duration. Previous trichoscopic descriptions of this condition have included yellow dots, black dots, empty follicular openings, short regrowing hairs, and dystrophic hairs, (all findings shared with active alopecia areata). Other previously described features include yellow structureless areas and yellow dots with ‘three-dimensional’ structure imposed over dystrophic hair shafts. This group found that, in their small cohort of patients, some trichoscopic features seemed to correlate with disease severity and duration. Patients presenting with a high degree of clinical inflammation showed empty follicular openings, yellow dots and black dots compared with patients with a low degree of inflammation. Three patients with longstanding disease showed a higher number of yellowish/whitish backgrounds. They suggest that further investigations should focus on assessing reliability of trichoscopy in identifying early and mild forms to address prompt treatment capable of preventing scarring and permanent hair loss.
CED – all relevant articles from the December/January journals were reported on in the November 2017 journal club
JAAD – no research articles for the January 2018 issue.
Clinical Pearl: The water-drop test for the diagnosis of koilonychia. Authors Khatiya Chelidze, BA, Shari R. Lipner, MD, PhD. Department of Dermatology, Weill Cornell Medicine, Cornell University, New York, New York.
Koilonychia is a common concave nail disorder giving rise to a spoon shaped nail with a central depression (derivation from the Greek for spoon “Koilos”). Dermatological causes are varied and include alopecia areata, psoriasis and lichen planus. Other medical causes include iron deficiencies, thyroid disorders, diabetes, genodermatoses and trauma. Although the diagnosis can be made on clinical examination, the changes can be subtle. The authors suggest the water drop test for the diagnosis of koilonychia where a 1ml syringe is used to place a few drops of water on the nail plate. In patients with normal or convex nail curvature the water will quickly fall off. However, in nails with concave curvature the water will stay on the nail plate, thereby assisting with diagnosis of koilonychia.
JEADV
Digit preserving surgery of subungual melanoma: a case series using vacuum assisted closure and full-thickness skin grafting. Authors D. Crisan,J. Gülke,C. Janetzko,S. Kastler,N. Treiber,K. Scharffetter-Kochanek,L.A. Schneider.
This letter to the editor presents a case series of an alternative surgical method to complete digital amputation in the management of alcrolentiginous melanoma. This is the second most common nail organ tumour and frequently affects the thumb or great toe. These digits are especially important in terms of function therefore, preservation is vitally important where possible (Loss of function of the thumb is associated with a loss of function of 40% of the entire hand).
Although digit amputation remains the gold standard, an alternative is to resect the tumour with distal phalanx preservation. These resections produce 3rd degree defects similar to avulsion injuries. There is therefore a need for temporary coverage and the authors advocate the use of vacuum-assisted closure (VAC) therapy. They propose that this provides a faster granulation than normal moist wound therapies. They tested their technique in 7 patients (four men, three women, age: 38–81 years, median 64), five confirmed melanoma in situ, one pT1a and one pT1b melanoma. In six patients, the primary tumour was located on the fingers (3xD4, 3xD1), in one case at big toe. All patients underwent the same surgical procedure. Two patients had to be amputated secondarily, one because of an injury to the joint distal interphalangeal joint capsule of the toe and the other in order to achieve required safety margins for in situ melanoma with poor demarcation on D4. The other five patients went on to full-thickness skin grafting after nail bed conditioning with the vacuum technique. All five patients achieved a completely healed skin graft and good cosmetic and functional results in the end. Six days after grafting, the patients started physiotherapy again to improve digital and joint mobility. The stitches were removed stepwise 10 and 14 days after surgery. VAC therapy achieved a sufficient granulation tissue for skin grafting on the initially uncovered bone surface with a median of 14 days (range 8–21). After a rehabilitation phase of 6 weeks, all five patients could resume normal activity. In a follow-up programme of 12 months, no local recurrence in these seven patients was seen.
JAMA
Dermatology Clinico-pathological challenge: Facial Papules in a Patient with Lichen Planopilaris
Athena J. Manatis-Lornell, BA1; Maryanne M. Senna, MD1
A woman in her 50s with biopsy-proven scalp lichen planopilaris (LPP) presented with an increasing number of slightly pruritic facial papules that coincided with the start of her hair loss condition. She denied a history of severe acne or other inflammatory skin disorders. The patient had no health problems and only had a distant medical history of an appendicectomy and an oophorectomy. The only medication she was taking was hydroxychloroquine 200 mg twice daily that was initiated as treatment of her LPP and did not improve the appearance or symptoms of her facial papules. On physical examination, she had numerous 1-mm skin-colored grouped monomorphic noninflammatory papules on the bilateral temples, the bilateral cheeks, and the chin. A 3-mm punch biopsy specimen was obtained for histopathologic examination of a representative lesion on the right chin.
Facial papules in Frontal Fibrosing Alopecia were clinically suspected. These are an increasingly recognised feature of facial vellus hair involvement in patients with FFA. Illustrating the importance of always keeping an open mind this patient’s pathology returned showing features consistent with miliary osteoma cutis. A second biopsy of a facial papule also showed osteoma cutis. The patient underwent a number of bloods including TSH, PTH, Vitamin D levels, calcium and phosphate. The only abnormality detected was a slightly elevated PTH level with no concerning underlying cause and not requiring treatment.
Facial Miliary osteoma cutis is a rare condition resulting in tiny deposits of bone fragments in the dermis. It presents with skin coloured papules that can be pruritic or asymptomatic. Often the patient presents due to cosmetic concerns. The lesions are thought to be either primary, or secondary to other inflammatory conditions. There is no agreed best treatment, however localised surgical excision, topical retinoids, dermabrasion and laser have all been used.