Nail article:
1. Hwang J, Ricardo J, Lipner S. Efficacy and Safety of Nail Psoriasis Targeted Therapies: A Systematic Review. Am J Clin Dermatol (2023). doi.org/10.1007/s40257-023-00786-4
Summary:
Nail psoriasis can have a significant impact on quality of life. Treatments range from topical medications, nail matrix/bed injections and systemic and biological therapies. There are a lack of clinical trials specifically measuring nail outcomes as primary endpoints.
This systematic review helps capture data from biologic and small molecule inhibitor studies for psoriasis, focusing upon efficacy and safety of therapies for nail psoriasis.
The authors included 68 studies encompassing 15 targeted therapeutic agents for nail psoriasis. These included TNF-alpha inhibitors (adalimumab, infliximab, etanercept, certolizumab, golimumab), IL-17 (ixekizumab, brodalumab, secukinumab), IL-12/23 inhibitors (ustekinumab), IL-23 inhibitors (guselkumab, risankizumab, tildrakizumab), PDE-4 inhibitors (apremilast), and JAK inhibitors (tofacitinib). All agents demonstrated statistically significant improvements in nail outcome scores (nail psoriasis severity index and modified nail psoriasis severity index) compared with placebo or baseline values at weeks 10-16 and weeks 20-26 with some including up to week 60. Specifically, head-to-head trials show superior efficacy for ixekizumab over adalimumab and ustekinumab, as well as brodalumab over ustekinumab. Safety data was in keeping with known profiles and largely acceptable.
Limitations included difficulties in comparing studies due to design/trial phase, scoring methods for nail disease, endpoints and sample sizes. Importantly most studies did not report long-term follow-up which is important due to the slow rate of nail growth and focused solely on fingernails.
Overall this is a useful systemic review, demonstrating that overall, multiple biologics and small molecule inhibitors are effective and safe for treating nail psoriasis and helps guide clinicians in terms of choice in patients with significant nail disease.
Hair articles:
1. Ogechi E, Shivali D, Balaji J, Kristen K, Maryanne S. Drug-induced alopecia areata: A systematic review. JAAD (2023) https://doi.org/10.1016/j.jaad.2023.05.022.
Summary:
Most cases of alopecia areata are idiopathic, however several triggers have been reported including medications. This systematic review helps capture the published medications which have been associated with de-novo alopecia areata and analyses outcomes of management.
The authors included 66 articles which were of generally lower quality including case reports, case series and retrospective studies. 30 drugs associated with de-novo alopecia areata were found. 66% of cases were associated with monoclonal antibodies; specifically dupilumab and TNF-a inhibitors (adalimumab, infliximab, etanercept, golimumab). Around half of patients discontinued the relevant drug and nearly all had regrowth within 9 months regardless of additional treatment. The rest who continued the drug with no additional treatment had no/minimal re-growth, but those opting for additional treatment had regrowth within 9 months.
Limitations included the authors limiting data gathering to one database (PubMed) and vaccinations were not mentioned or included which would have made important and interesting additional data. Patients with a prior history of alopecia areata were excluded which may have missed patients with flares due to new medications, however due to the unpredictable nature of the condition causality (rather than association) is difficult to determine.
Overall this review highlights the medications which are associated with alopecia areata, with the majority of cases relating to TNF-a monoclonals and dupilumab. This is a useful reminder for the clinicians of the association and the outcomes appears favourable if the medication is stopped and/or additional treatments given.
2. Plante J, Valdebran M, Forcucci J, Bosland J, Elbendary A, Jaiswal R, Elston D. Perifollicular Microscarring in Alopecia Areata and Pattern Hair Loss. Am J Dermatopathol. (2023). doi: 10.1097/DAD.0000000000002398
Summary:
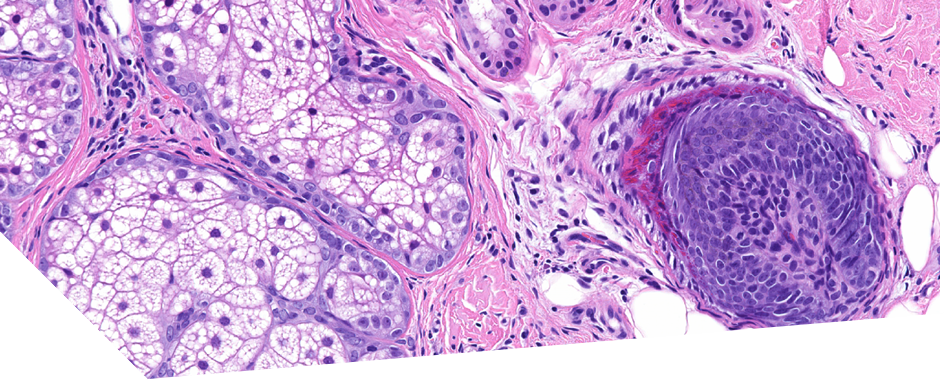
Alopecia areata and patterned hair loss are non-scarring forms of alopecia. Previous reports have demonstrated perifollicular fibrosis in some biopsies. Previous reports have hypothesised this is related to chronicity of the condition. This study aimed to retrospectively analyse the frequency of focal perifollicular fibrosis and true microscarring with loss of elastic tissue in biopsy samples in patients with alopecia areata and patterned hair loss.
The authors included 62 cases comprising of 20 alopecia areata cases and 42 patterned hair loss cases from their tertiary referral centre. 5 cases of alopecia areata (25%) demonstrated perifollicular fibrosis and true microscarring when assessed using Verhoeff Van Gieson staining. For patterned hair loss 12 (28.6%) demonstrated perifollicular fibrosis and true microscarring when assessed using Verhoeff Van Gieson staining.
Limitations included low numbers of patient samples and the retrospective nature of the study. The authors attempted to use fluorescence microscopy to assess for true microscarring but this had low sensitivity during analysis for alopecia areata cases so did not use it for patterned hair loss samples, hindering comparison. Strengths included using two independent reviewers to review the histology, but blinding was not used. The chronicity of the condition in patients providing samples was not documented which is a major flaw.
Overall this study demonstrates a high rate of focal perifollicular fibrosis and true microscarring in both conditions, however the study had significant design limitations. Importantly the disease duration of the condition should be included in further studies and documentation of co-existing clinical features of a concurrent scarring alopecia, as two forms (scarring and non-scarring) of alopecia can co-exist. Clinicians should be aware of this phenomenon in classically non-scarring alopecia when reviewing histopathology with clinical findings.
3. Shen Y, Sun J, Zhu Y, Chen Y, Hu Y, Luo H, Song X. Effect of fractional laser alone or in combination on alopecia areata: A systematic review and meta-analysis. J Cosmet Dermatol. (2023). doi: 10.1111/jocd.15630
Summary:
The hair follicle is the target of treatment in alopecia areata and delivery of topical treatments are limited by the stratum corneum and it’s other stroma. Fractional lasers can provide non/minimally invasive drug delivery channels to improve transdermal drug absorption. Previous studies have concluded differing opinions on its effectiveness in alopecia areata.
This systematic review looked at the evidence for fractional lasers alone or in combination with other therapies to treat alopecia areata.
14 studies were included including 10 randomised controlled studies which included 815 patients. Lasers used included 10 600 nm ultra-pulsed fractional CO2 laser, 1565 nm non-ablative fractional laser, 1550 nm non-ablative fractional laser, 2940 nm fractional erbium yttrium aluminum garnet laser, and three used non-ablative laser. Duration of 12 weeks of treatment was most common with treatments ranging between every 2-6 weeks. Treatment response was defined as newly regenerated hair >50%.
Combination treatment of fractional laser increased incidence of achieving ≥50% new hair with both minoxidil (by 1.32-fold) and topical steroid (by 1.39 fold), with greater efficacy compared with either drug alone. Fractional laser alone was also effective in the treatment of alopecia areata (10.33 times greater compared with no treatment) and more effective than topical steroid alone (by 1.85 times). Comparison of fractional laser to other comparable physical treatments (308 excimer light, neodymium: yttrium aluminum garnet (Nd: YAG), and cryotherapy) did not find greater effectiveness. Fractional lasers were not associated with major significant adverse events.
Limitations included a small number of studies being included, which were often at a high risk of bias. Difficulties in comparisons also resulted from different durations and number of treatment and treatment protocols. The authors were not able to determine which type of fractional laser was most beneficial .
Overall there is limited data, but trends towards improvement when combining fractional laser with topical minoxidil / steroids. Fractional laser did not seem to differ significantly when compared to comparable treatments. This data may provide clinicians with other safe treatment options in patients who are not suitable for, or do not want systemic medication.
4. Abdi W, Dow Y, Blalock T. Ethically conducting hair examinations among individuals with hijabs. JAAD (2023) doi.org/10.1016/j.jaad.2023.05.020
Summary:
This short letter in the Ethics Journal Club explores the hijab in the Muslim faith and the importance of clinicians to address this religious practice during clinical examiantion with humility and cultural competency. Adaptive methods to examination may include detailed advice on how to take pre-visit photographs or offering photography within a private area with a gender-concordant team member if desired. Practicing culturally sensitive communication is important to honour boundaries and optimise patient comfort.
5. Onamusi T, Larrondo J, McMichael A. Clinical factors and hair care practices influencing outcomes in central centrifugal cicatricial alopecia. Arch Dermatol Res (2023). https://doi.org/10.1007/s00403-023-02630-5
Summary:
This retrospective study analysed data from 100 patient’s medical notes with CCCA who had received treatment for at least 1 year and assessed any possible associations of treatment outcomes with patient characteristics. Treatments included topical and intralesional steroids, topical minoxidil and oral doxycycline. Improvement was assessed using photographs looking at hair density and graded according to a Central Scalp Photography Scale. Statistical methods included logistic regression was used with univariate analysis.
Main findings included; a higher odds of improvement in disease in patients without a history of thyroid disease, using metformin for diabetes control, using hooded dryers, wearing natural hairstyles and having no other physical signs except cicatricial alopecia. Scaling and pustules were found to be associated with a higher rate of worsening of disease.
Limitations included not all patients having a biopsy confirmed diagnosis of CCCA. No blinding used or information about who/how many assessors reviewed the photographs, a small sample size with wide confidence intervals, a retrospective design and the study being prone to observer bias.
Overall, this study highlights that clinicians should consider other clinical signs such as pustules and scaling as negative predicted factors for improvement. Patient’s comorbidities when treating CCCA such as associated thyroid disease and diabetes should be reviewed and treatment optimised. Hairstyles and hair care practices have been implicated in CCCA with conflicting data. This study was in keeping with previous reports suggesting that natural hairstyles had a higher chance of improving, however the association with use of hooded driers remains unexplained.
6. Johnston L & Poelman S. Upadacitinib for management of recalcitrant alopecia areata: A retrospective case series. JAAD Case Rep. (2023) doi: 10.1016/j.jdcr.2023.02.019
Summary:
This retrospective case series reports 3 cases of recalcitrant alopecia areata which were successfully treated with upadacitinib. 2 females (37 and 62 years old) and 1 male (27 years old) were included. Two patients had comorbid atopic dermatitis. A variety of previous treatments had been trailed including topical agents and oral medications including prednisolone (n=1) and methotrexate (n=1). Upadacitinib was given at 30mg for 3-5 months, followed by 15mg for a further 3 months in one patient. All patients had complete hair regrowth on the scalp with improvement in other areas such as the eyebrows in 2 patients. The drug was well tolerated with 1 patient developing mild acne. One patient had an ophiasis pattern of AA which is particularly difficult to treat, and responded well to the JAK-inhibitor.
This case series highlights upadacitinib as another treatment option in refractory AA which appears to be well tolerated and effective.
7. Shadi Z. Compliance to Topical Minoxidil and Reasons for Discontinuation among Patients with Androgenetic Alopecia. Dermatol Ther (Heidelb). (2023) doi: 10.1007/s13555-023-00919-x
Summary:
Topical minoxidil is a commonly used medication for androgenetic alopecia but use can be limited by side effects.
This retrospective study analysed 400 patients with androgenetic alopecia who were prescribed topical minoxidil 2% or 5% in the last 5 years. Demographic factors, previous treatments, minoxidil parameters, total duration or use and side effects were analysed.
66.5% of patient were female with a mean age of 32.4 years old. Most patients did not receive any previous treatment for their hair loss. A high proportion of patients discontinued minoxidil (86%) and most used the treatment for under 6 months. Discontinuation was not associated with sex, age or previous treatment. Patients who reported improvement and had used the treatment for longer were less likely to discontinue. Patients who reported baby hair or no efficacy were more likely to discontinue treatment. Patients reporting an adverse effect (46%) from the medication were more likely to discontinue treatment. The 5 most common adverse effects in order included itching, facial hair growth, accelerated hair loss, seborrhoea exacerbation and headache. However the most common reason for discontinuation reported was lack of compliance rather than an unsatisfactory result, but side effects increased the likelihood of cessation threefold.
Limitations to this study included the lack of analysis into other barriers which may impact poor compliance to treatment including socioeconomic factors and difficulties in treatment application. Patient knowledge and expectations of the treatment efficacy, as well as frequency of use would also be important to assess.
Overall this study highlighted that use of topical minoxidil is limited by low compliance even in the absence of adverse effects and most patients discontinue within the first few months of treatment. Important take-home messages include the importance of patient education regarding adverse effects and treatment duration recommendations, including that cessation of treatment is likely to lead to reversal of any improvement.